In the modern world, the resonance of disease with cervical osteochondrosis can hardly be overestimated. Osteochondrosis in the cervical area is more common than in other vertebral areas. Almost everyone over the age of twenty -five has this disease, to one degree or another.

Cervical osteochondrosis develops primarily due to an inactive lifestyle, which is primarily facilitated by a person’s historical transition from physical labor to mental labor, which, even at a moderate level, is accompanied by work in a sitting position.
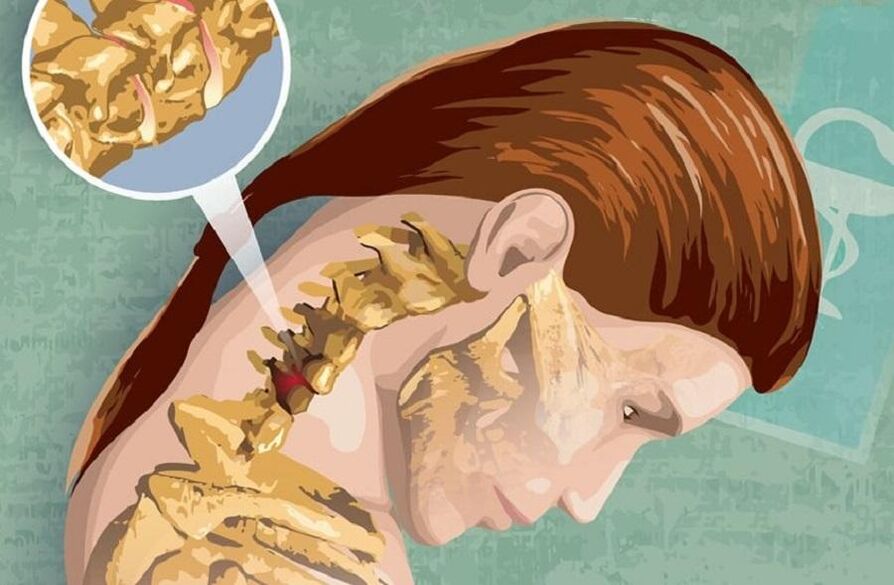
Cervical osteochondrosis is a degenerative-dystrophic disease of the cervical spine, leading to damage to the intervertebral disc, which is common in general for osteochondrosis. Since this part of the spine is, by its nature, relatively mobile, but at the same time vulnerable due to the underdeveloped muscular corset, therefore, any negative impact on the neck or back affects the cervical area first. Due to the fact that degenerative changes most often develop in the most mobile part of the vertebra, precisely the nerve endings at the C5 level. . . C7 most often suffers in the cervical region.
Because the symptoms of cervical osteochondrosis are so controversial, they are not always considered simply as symptoms of the disease, which often leads to seeking help from specialists in other medical fields. Let us consider them in more detail.
symptoms
Due to the fact that the cervical spine is relatively dense, compared to its other departments, even slight tension on the neck muscles or displacement of the cervical spine vertebrae can cause compression or pinching of nerve roots, which can also affect vessels located in this department. Well, osteophytes - bone growth, in folk treatment called "salt deposition" and formed in the course of disease progression with cervical osteochondrosis, lead, consequently, only to a significant deterioration in the course of the disease.
The clinical manifestations of cervical osteochondrosis disease, that is, its symptoms, can be divided into reflex symptoms and radicular symptoms of cervical osteochondrosis.
Reflex symptoms of cervical osteochondrosis
Reflex symptoms of cervical osteochondrosis include the so -called "lumbago", which is expressed in the appearance of a sharp sharp pain in the neck, and significantly increases with any movement. Given this, patients often assume some type of forced, most comfortable, head position. In addition, it is quite possible that a common "crunch" occurs when turning or other head movements.
With cervical osteochondrosis, patients often experience headaches that are compressive in nature and radiate to the eyeballs or the temporal part of the head. In addition, sometimes at the same time, the acuity of visual perception may decrease, as if "everything is floating in front of the eyes. "
Vertebral artery syndrome can also develop, when the nerve plexus is irritated, which very often, due to dizziness in patients, is mistakenly diagnosed as a violation of cerebral blood circulation. Symptoms of such cervical osteochondrosis can manifest with sudden head movements and be complicated by nausea and the possibility of vomiting.
In addition to the above, reflex symptoms of cervical osteochondrosis also include cardiological syndrome, in which there is a sensation similar to an angina attack. But manifestations such as symptoms of osteochondrosis are usually combined with a complex of other symptoms of the disease, so it usually does not cause difficulties in making a correct diagnosis.
Radicular symptoms of cervical osteochondrosis
The radicular symptoms of cervical osteochondrosis, as a rule, appear due to compression of the nerve endings of the spine - the roots. In this case, the sensory disturbances that affect motor function depend entirely on the specific nerve root of the injury, namely:
- C1 - decreased sensitivity in the back of the head;
- C2 - occurrence of pain in the parietal or occipital region of the head;
- C3 - violation of sensitivity and the appearance of pain in the neck, in which the roots of the spine are injured, with a very possible violation of speech function, due to loss of sensitivity of the tongue and control over it;
- C4 - the appearance of pain and decreased sensitivity in the dorsal humeroscapular region, as well as pain in the heart and liver area, with a simultaneous decrease in neck muscle tone and possible respiratory disorders of respiratory function;
- C5 - decreased sensitivity and pain on the outer shoulder surface;
- C6 - pain radiating from the cervical region to the scapula, outer shoulder surface, forearm, and further from the wrist to the thumb;
- C7-same pain as in C6, but radiating from the scapula to the posterior shoulder surface, and further from the forearm to the 2nd to 4th fingers, with decreased sensitivity in the pain area;
- C8 - decreased sensitivity and pain from the neck to the shoulders, and then from the forearm to the little finger.
Treatment

Cervical osteochondrosis is a relatively complex and very unpleasant disease, the treatment of which requires consistency, duration and stage. Therapeutic treatment of cervical osteochondrosis, first of all, aims at the complete cessation of the painful symptoms of cervical osteochondrosis and the elimination of inflammation in the neck area affected by the disease.
Patients, in the treatment of cervical osteochondrosis, are treated with classic analgesics, such as analgin, ketorol or baralgin. Although recently non-steroidal anti-inflammatory drugs have also been widely popular in the treatment of cervical spine osteochondrosis, effectively relieving pain and reducing inflammatory activity.
Among other things, in the treatment of cervical osteochondrosis, chondroprotectors are also used, which slow down the process of destruction of cartilage tissue and, according to many experts, also contribute to their regeneration process. In addition, patients are prescribed the use of B vitamins, which improve metabolic processes in the patient's body.
But the use of external gels or ointments for the treatment of cervical osteochondrosis is ineffective, but makes sense, because in the process of rubbing it into the skin, additional massage of the cervical spine area is performed.
Physiotherapy procedures are also combined with traditional medicine treatment of cervical osteochondrosis, and in particular, the use of magnetotherapy through special medical devices that have gained due popularity among specialists and patients is highly effective. Also used, in addition to the above, are also therapeutic massages, physiotherapy exercises and manual therapy. But, in cases of severe disease, surgical intervention may also be required.
Prevention of cervical osteochondrosis
By itself, the prevention of cervical osteochondrosis is not difficult. Recommended:
- maintain an active and healthy lifestyle,
- sports, or at least morning exercise,
- efficient organization in the workplace,
- adherence to work and rest regimes,
- during prolonged work in a sitting position - during working hours, warm up several times and ensure correct head position and posture while working.
It is also important to choose comfortable pillows and mattresses for sleeping. But for those who already suffer from this disease, the daily use of orthopedic products specifically for a comfortable sleep is highly recommended.

























